|
Coronary MRA is the most difficult of all vascular studies to perform well. The coronary arteries are small (2-4 mm), tortuous, and move in a complex fashion with each heart beat and with respiration. Recent advances and clinical success with coronary CTA have somewhat dampened enthusiasm and clinical applications for coronary MRA, though research continues on both.
Coronary MRA may be useful in the following situations: 1) identification of anomalous coronary arteries; 2) detection of coronary artery ectasia or aneurysms in Kawasaki disease; 3) assessing the patency of coronary artery bypass grafts; and 4) demonstration of stenosis of native coronary arteries, especially in their proximal portions.
|
The complex motion of the heart during its contraction/relaxation cycle requires EKG-triggering and segmented image acquisition. A quick scout axial cine MRI study should be obtained to determine the pattern of gross cardiac motion and hence the optimal window for imaging. For most patients mid-to-late diastole is a particularly favorable time where gross motion is minimized and coronary flow is high. In pediatric patients with fast heart rates, however, the best time may be late systole. In patients of any age with rapid or irregular heart beats, the β-blocker drugs may prove useful. Coronary MRA is likely to be unsuccessful in patients with frequent intruding arrhythmias.
Compensation for respiratory motion is best performed using a navigator beam oriented perpendicular to the right hemidiaphragm. The navigator pulse is interleaved with the cardiac MRA sequence and permits image acquisition only when the diaphragm is within a predefined tolerance band near its end-expiratory position. The use of navigators improves patient comfort and tolerance since it allows free-breathing during what is often a somewhat lengthy (10+ minute) coronary MRA study.
|
Pulse sequences for coronary MRA include black blood and bright blood techniques. Black-blood 2D techniques are relatively easy to perform and may be perfectly adequate if only limited information is needed, such as the origins of coronary arteries.
For general coronary MRA, however, non-contrast bright blood techniques are currently the most popular. Two strategies are available: 1) a single 3D-volumetric sequence covering the entire heart, or 2) two shorter duration slab acquisitions targeting the right and left coronary systems respectively.
|
For optimal spatial resolution of the entire coronary tree, a (nearly) isotropic 3D data set is required. The best results to date have been obtained using segmented b-SSFP sequences with T2-magnetization preparation and frequency-selective fat suppression. Parallel imaging is mandatory to keep acquisition times in a tolerable range. Pre-scan shimming is also recommended. A commercially available coronary artery MRA sequence offered on Philips systems is illustrated below.
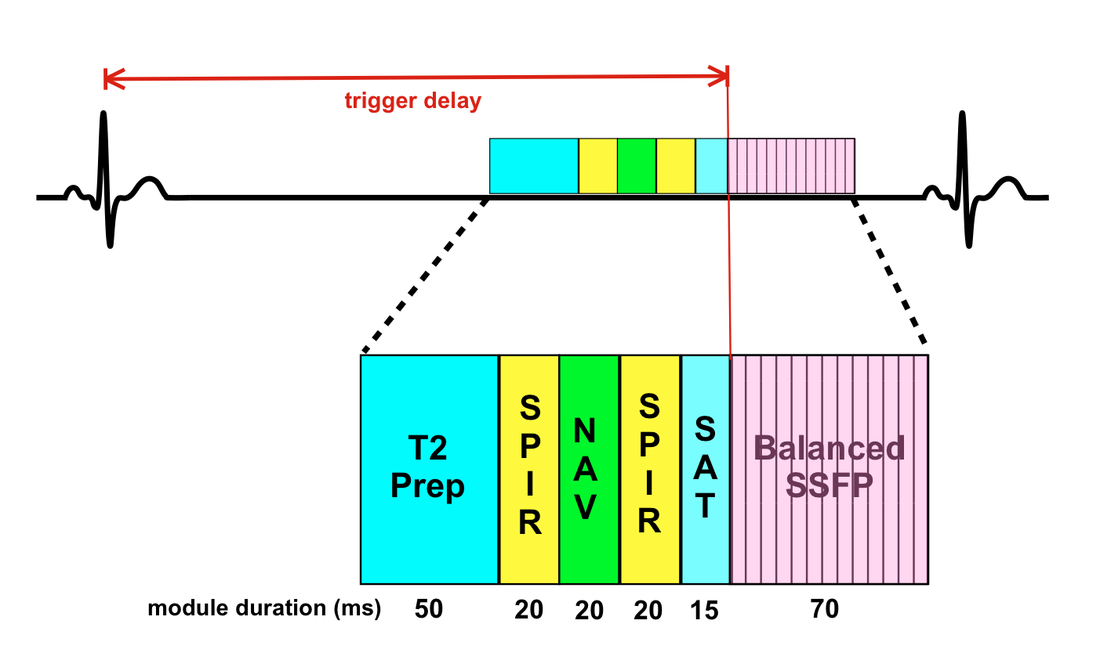
Coronary MRA pulse sequence offered by Philips. The T2 Prep module is a short train (1-4) of nonselective RF-pulses to suppress tissues with short T2 values and accentuate blood. Two SPIR fat suppression pulses (yellow) are used. The first suppresses fat along the navigator (NAV) beam to improve its stability, while the second suppresses epicardial fat surrounding the coronary arteries. A spatial saturation (SAT) pulse is placed on the chest wall for fold-over suppression. Image acquisition (pink) occurs during late diastole. A balanced-SSFP readout is typically employed, but other methods (turbo-SE, EPI, hybrid GRE-EPI) are also possible. In this example a radial profile order beginning at the center of k-space with clipping of k-space corners is used ("k-space shuttle"), so the trigger delay is defined from the R-wave to the start of data acquisition.
 Multiplanar reformation of 3D data set shows proximal course(s)
Multiplanar reformation of 3D data set shows proximal course(s) of the right and left coronary arteries.
Following image acquisition multiplanar and curved reformations of the 3D (volumetric) data set are required to display the course(s) of the coronary arteries. An example is shown left.
Promising future developments include: 1) coronary artery MRA at 3T where improved spatial resolution is possible due intrinsically higher signal-to-noise; 2) the use of intravascular contrast agents; 3) compressed sensing; 4) deep learning reconstruction methods; and 5) phase-contrast imaging to quantify blood flow in the proximal coronary arteries. Head-to-head comparison studies will be needed to determine the role(s) coronary artery MRA will ultimately play in evaluating patients with known or suspected heart disease, especially in light of the great successes now being touted for coronary CTA.
Promising future developments include: 1) coronary artery MRA at 3T where improved spatial resolution is possible due intrinsically higher signal-to-noise; 2) the use of intravascular contrast agents; 3) compressed sensing; 4) deep learning reconstruction methods; and 5) phase-contrast imaging to quantify blood flow in the proximal coronary arteries. Head-to-head comparison studies will be needed to determine the role(s) coronary artery MRA will ultimately play in evaluating patients with known or suspected heart disease, especially in light of the great successes now being touted for coronary CTA.
Advanced Discussion (show/hide)»
No supplementary material yet. Check back soon!
References
Bluemke DA, Achenbach S, Budoff M, et al. Noninvasive coronary artery imaging: magnetic resonance angiography and multidetector computed tomography angiography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention, and the Councils on Clinical Cardiology and Cardiovascular Disease in the Young. Circulation 2008; 118:586-606.
Bustin A, Ginami G, Cruz G, et al. Five-minute whole-heart coronary MRA with sub-millimeter isotropic resolution, 100% respiratory scan efficiency, and 3D-PROST reconstruction. Magn Reson Med. 2019;81:102–115. (innovative 3D technique involving bSSFP spiral acquisitions with under sampling that works well in healthy volunteers so far)
Hamdy A, Ishida M, Sakura H. Cardiac MR assessment of coronary arteries. CVIA 2017; 1:49-59.
Sakuma H, Ichikawa Y, Suzawa N, et al. Assessment of coronary arteries with total study time of less than 30 minutes by using whole-heart coronary MR angiography. Radiology 2005; 237:316-321.
Stuber M, Weiss RG. Coronary magnetic resonance angiography. J Magn Reson Imaging 2007; 26:219-234.
Bluemke DA, Achenbach S, Budoff M, et al. Noninvasive coronary artery imaging: magnetic resonance angiography and multidetector computed tomography angiography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention, and the Councils on Clinical Cardiology and Cardiovascular Disease in the Young. Circulation 2008; 118:586-606.
Bustin A, Ginami G, Cruz G, et al. Five-minute whole-heart coronary MRA with sub-millimeter isotropic resolution, 100% respiratory scan efficiency, and 3D-PROST reconstruction. Magn Reson Med. 2019;81:102–115. (innovative 3D technique involving bSSFP spiral acquisitions with under sampling that works well in healthy volunteers so far)
Hamdy A, Ishida M, Sakura H. Cardiac MR assessment of coronary arteries. CVIA 2017; 1:49-59.
Sakuma H, Ichikawa Y, Suzawa N, et al. Assessment of coronary arteries with total study time of less than 30 minutes by using whole-heart coronary MR angiography. Radiology 2005; 237:316-321.
Stuber M, Weiss RG. Coronary magnetic resonance angiography. J Magn Reson Imaging 2007; 26:219-234.
Related Questions
How can navigators track heart position if placed on the diaphragm?
What is SPIR and how does it compare to other fat suppression methods?
How can navigators track heart position if placed on the diaphragm?
What is SPIR and how does it compare to other fat suppression methods?