The evolution of subarachnoid hemorrhage (SAH) on MRI differs significantly from hemorrhages confined to the brain parenchyma. Clots in the subarachnoid space are usually small, multiple, and diffuse. They are exposed to, and mixed with, cerebrospinal fluid, which has high pO2 values. High ambient oxygen levels mean that SAH will evolve more slowly than parenchymal hematomas on MRI.
In the hyperacute phase of SAH, slight shortening of T1 occurs due to the increased protein and new cellular content within cerebrospinal fluid (CSF). This produces a “dirty CSF” appearance on T1-weighted and T2-FLAIR images, while T2-weighted images are generally not affected. It should be noted that small degrees of SAH in this phase may be difficult to detect by MRI, leaving CT as the preferred diagnostic modality for the hyperacute clinical scenario.
T2/T2*-shortening occurs with transition to deoxyhemoglobin, but decreased signal may be difficult to appreciate on T2-weighted images unless the hemorrhage is massive or collects in the ventricular system. Susceptibility-weighted (SW) or gradient echo (GRE) images may be better for SAH detection during this phase, although T2-FLAIR remains an important diagnostic sequence at all stages.
Transition to methemoglobin with shortening on T1-weighted images is often delayed to late in the first week after SAH. In mild SAH this phase may never be seen as the hemoglobin may be diluted, resorbed, or dispersed before methemoglobin formation occurs. If present, however, the T1-shortening from methemoglobin may allow diagnosis of SAH at a time when CT images have returned to normal. Even though T1 shortening occurs, T2-FLAIR may still be superior for detection even in this later period.
T2/T2*-shortening occurs with transition to deoxyhemoglobin, but decreased signal may be difficult to appreciate on T2-weighted images unless the hemorrhage is massive or collects in the ventricular system. Susceptibility-weighted (SW) or gradient echo (GRE) images may be better for SAH detection during this phase, although T2-FLAIR remains an important diagnostic sequence at all stages.
Transition to methemoglobin with shortening on T1-weighted images is often delayed to late in the first week after SAH. In mild SAH this phase may never be seen as the hemoglobin may be diluted, resorbed, or dispersed before methemoglobin formation occurs. If present, however, the T1-shortening from methemoglobin may allow diagnosis of SAH at a time when CT images have returned to normal. Even though T1 shortening occurs, T2-FLAIR may still be superior for detection even in this later period.
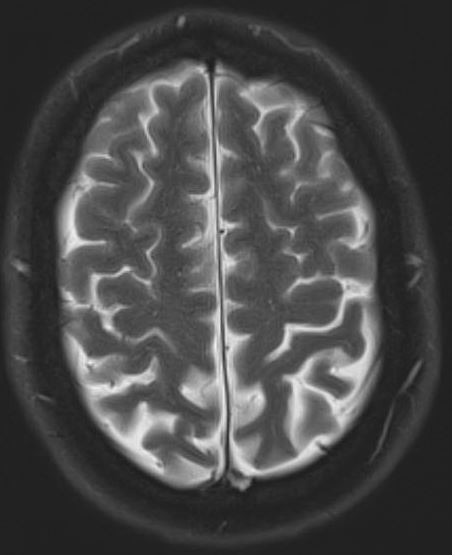
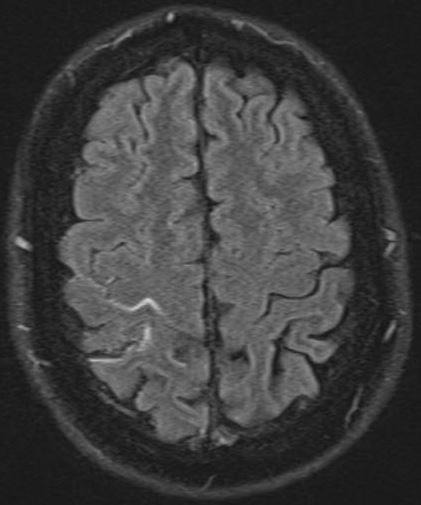
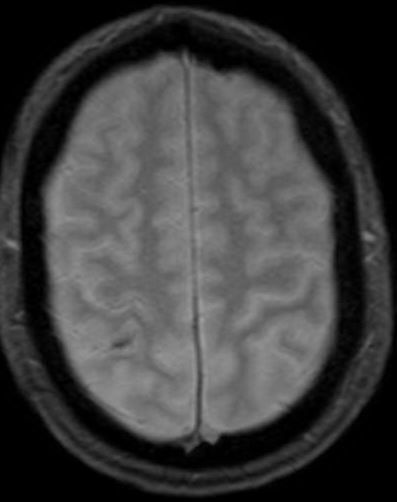
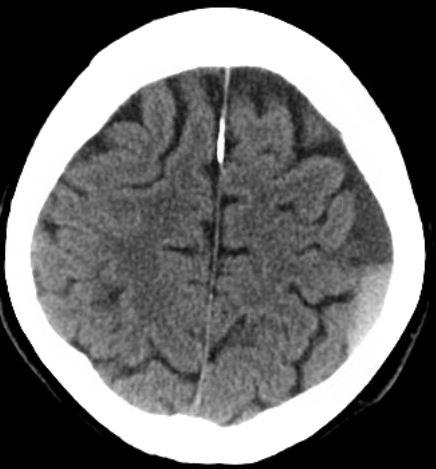
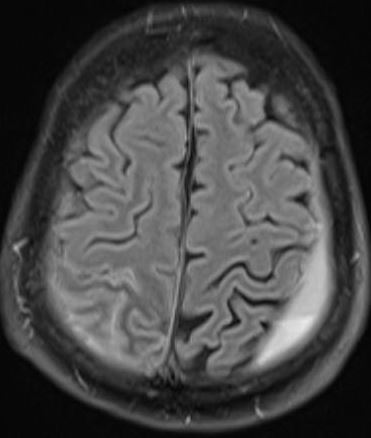
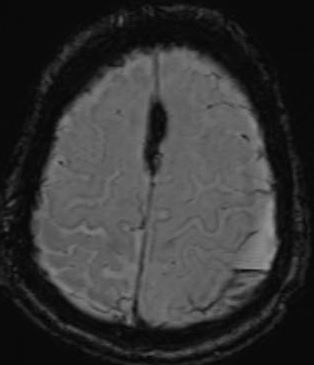
The two cases below show how certain MR sequences, especially T2-FLAIR, Gradient/Susceptibility, and diffusion-weighted imaging may reveal subarachnoid hemorrhage when CT is negative or equivocal.
Case 1 (Above). CT and MRI 5 days after subarachnoid hemorrhage. CT and T2-weighed MRI are negative. T2-FLAIR and GRE images show abnormal signal within right parietal sulci.
Case 2 (below). CT and MR 2 days after head trauma. A small left-sided subdural hemorrhage with fluid-fluid level is well seen on all images. The subarachnoid hemorrhage in right parietal region is difficult to appreciate on CT but clearly visible on T2-FLAIR, DWI, and SWI images.
Finally, large or repeated subarachnoid hemorrhages may leave their characteristic signature by hemosiderin deposition on the meninges and brain's exterior. This is known as superficial siderosis, characterized by very low signal on T2 and T2* images outlining the brain's surfaces. A similar phenomenon may be seen along the serosal surfaces of joints following hemarthroses.
Advanced Discussion (show/hide)»
No supplementary material yet. Check back soon!
References
Bradley WG Jr, Schmidt PG. Effect of methemoglobin formation on the MR appearance of subarachnoid hemorrhage. Radiology 1985; 156:99-103.
Bracchi M, Savoiardo M, Triulzi F, et al. Superficial siderosis of the CNS: MR diagnosis and clinical findings. AJNR Am J Neuroradiol 1993; 14:227-236.
da Rocha AJ, da Silva CJ, Gama HP, et al. Comparison of magnetic resonance imaging sequences with computed tomography to detect low-grade subarachnoid hemorrhage: role of fluid-attenuated inversion recovery sequence. J Comput Assist Tomogr 2006; 30:295-303.
Noguchi K, Ogawa T, Seto H, et al. Subacute and chronic subarachnoid hemorrhage: diagnosis with fluid-attenuated inversion recovery MR imaging. Radiology 1997;203:257–262
Rumboldt Z, Kalousek M, Castillo M. Hyperacute subarachnoid hemorrhage on T2-weighted MR images. AJNR Am J Neuroradiol 2003; 24:472-475.
Verma RK, Kottke R, Andereggen L, et al. Detecting subarachnoid hemorrhage: comparison of combined FLAIR/SWI versus CT. Eur J Radiol 2013; 82:1539-1545.
Bradley WG Jr, Schmidt PG. Effect of methemoglobin formation on the MR appearance of subarachnoid hemorrhage. Radiology 1985; 156:99-103.
Bracchi M, Savoiardo M, Triulzi F, et al. Superficial siderosis of the CNS: MR diagnosis and clinical findings. AJNR Am J Neuroradiol 1993; 14:227-236.
da Rocha AJ, da Silva CJ, Gama HP, et al. Comparison of magnetic resonance imaging sequences with computed tomography to detect low-grade subarachnoid hemorrhage: role of fluid-attenuated inversion recovery sequence. J Comput Assist Tomogr 2006; 30:295-303.
Noguchi K, Ogawa T, Seto H, et al. Subacute and chronic subarachnoid hemorrhage: diagnosis with fluid-attenuated inversion recovery MR imaging. Radiology 1997;203:257–262
Rumboldt Z, Kalousek M, Castillo M. Hyperacute subarachnoid hemorrhage on T2-weighted MR images. AJNR Am J Neuroradiol 2003; 24:472-475.
Verma RK, Kottke R, Andereggen L, et al. Detecting subarachnoid hemorrhage: comparison of combined FLAIR/SWI versus CT. Eur J Radiol 2013; 82:1539-1545.