Navigators are extra RF-pulses (with echoes) integrated into routine imaging sequences. By measuring the phase shift of navigator echoes, the positions of moving organs or structures can be monitored continuously during MR image acquisition.
|
Navigator pulses are typically applied so as to excite 1-dimensional beams or 2-dimensional planes of tissue. Although navigators may be placed over the heart directly, more commonly they are placed to intersect the right hemidiaphragm at its dome. Knowing the superior-inferior (SI) position of the diaphragm, the heart position can be indirectly calculated.
|
|
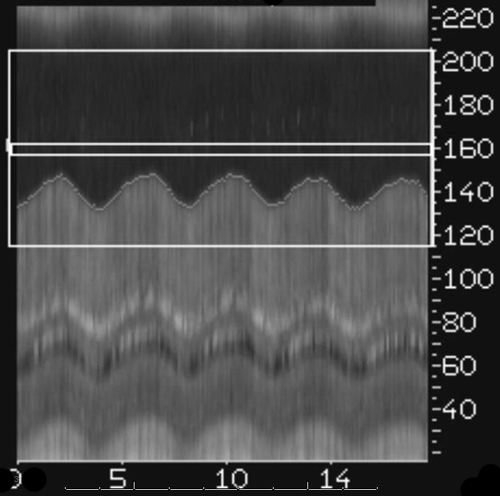
The echo signal returned by the navigator is reconstructed in the readout (motion) direction and displayed as lines of data along the beam direction. This technique is a form of line-scan imaging. It is also known as M-mode display since is equivalent to that used for viewing valve motion in M-mode echocardiography.
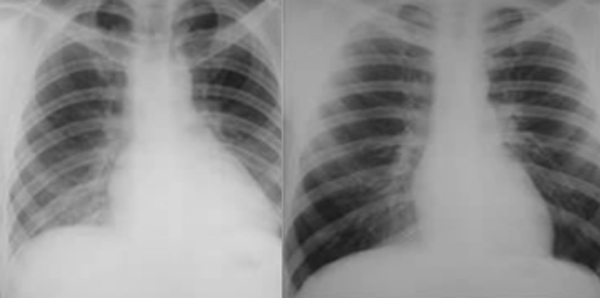
Automated software detects the diaphragmatic peaks and troughs of motion. The MR technologist defines an acceptance (gating) window that is typically on the order of ± 2.5 mm. The larger the window, the more time for image acquisition, but at the price of increased motion artifacts. The term navigator efficiency refers to the percentage of heartbeats over which data is acquired and is usually in the range of 30-50%.
|
In their simplest implementation described above, navigator echoes serve only as respiratory gating method. In a more advanced implementation (prospective adaptive motion correction) navigators can dynamically redefine the position of the imaging volume based on diaphragmatic position. The relationship is somewhat complex in that rotation and translation of the heart do not occur exactly in a 1:1 concordance with the diaphragm.
Empiric compensation factors have therefore been established to estimate cardiac motion as a function of diaphragm position. In the SI direction in normal-sized adults, for example, 10 mm of diaphragm movement translates to about 6 mm of movement of the superior margin of the heart, about 7 mm for the left anterior descending (LAD) coronary artery, and about 8 mm for the cardiac apex. The anterior-posterior (AP) movement of these structures is smaller and less variable, typically only about 2 mm for every 10 mm of diaphragm excursion. Left-to-right cardiac displacement with respiration is usually minimal and typically disregarded.
Although generic correction factors may be used, better results are obtained on a patient-by-patient basis. Alternatively, passing navigator beams directly through the heart obviates the need for indirect estimates, but is difficult to set up and monitor initially.
Although generic correction factors may be used, better results are obtained on a patient-by-patient basis. Alternatively, passing navigator beams directly through the heart obviates the need for indirect estimates, but is difficult to set up and monitor initially.
Advanced Discussion (show/hide)»
Methods where the navigator echo beam has been directed to the heart itself have been difficult to produce consistent results This is because the flowing blood in the ventricles creates complex phase shifts that complicate the navigator signal, making it difficult to extract cardiac wall motion as an independent variable. Some better success has been obtained by navigating to epicardial fat through the use of spectral-spatial pulses.
References
Ehman RL, Felmlee JP. Adaptive technique for high-definition MR imaging of moving structures. Radiology 1989; 173:255-263.
Nehrke K, Manke D. Advanced navigator techniques. Int J Bioelectromag 2000; 2(2) online at this link.
Nguyen TD, Nuval A, Mulukutla S, Wang Y. Direct monitoring of coronary artery motion with cardiac fat navigator echoes. Magn Reson Med 2003; 50:235-241.
Welch EB, Manduc A, Grimm RC et al. Spherical navigator echoes for full 3D rigid body motion measurements in MRI. Magn Reson Med 2002; 47:32-41.
Ehman RL, Felmlee JP. Adaptive technique for high-definition MR imaging of moving structures. Radiology 1989; 173:255-263.
Nehrke K, Manke D. Advanced navigator techniques. Int J Bioelectromag 2000; 2(2) online at this link.
Nguyen TD, Nuval A, Mulukutla S, Wang Y. Direct monitoring of coronary artery motion with cardiac fat navigator echoes. Magn Reson Med 2003; 50:235-241.
Welch EB, Manduc A, Grimm RC et al. Spherical navigator echoes for full 3D rigid body motion measurements in MRI. Magn Reson Med 2002; 47:32-41.
Related Questions
What are navigator echoes and how do they reduce motion artifacts?
What are navigator echoes and how do they reduce motion artifacts?