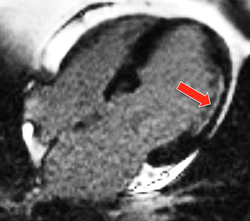
 Contrast enhancement along lateral wall
Contrast enhancement along lateral wall of LV at site of infarction.
Both normal and diseased myocardium will take up gadolinium contrast and exhibit enhancement. The rates of gadolinium accumulation and washout depend on multiple factors, including presence/type of heart disease, myocardial blood supply, heart rate, hematocrit, and renal function. Many diseases result in myocardial fibrosis with expansion of the extracellular compartment. As shown in the diagram below, the relative contrast enhancement between normal and diseased myocardium depends on the time after injection that imaging is performed.

|
1. Acute infarction with reperfusion. First pass imaging is normal, but delayed CE seen in segments where myocardial necrosis is present.
2. Acute infarction without reperfusion. This is known as microvascular obstruction (MVO), portending a worse prognostic outcome (heart failure, recurrent infarction, etc). First pass imaging demonstrates a low-signal (nonperfused) core. Late imaging may show either no or very weak delayed enhancement.
|
4. Chronic infarction. Characterized by myocardial thinning and fibrosis, first pass imaging is normal to slightly delayed while late contrast enhancement is seen. Note that acute from chronic myocardial infarction may be difficult to distinguish by contrast-enhanced CMR alone. A section of myocardial wall with greater than 50% thickness involved by enhancing scar or fibrosis is unlikely to recover contractile function following myocardial revascularization.
5. Hibernating myocardium. These areas have decreased function and blood flow but no dead cells. They have a normal appearance on early and delayed contrast imaging and good prognosis in response to revascularization. The term "viable myocardium" refers to myocardium that may recover contractile function following coronary artery revascularization.
 Patchy transmural enhancement in sarcoidosis
Patchy transmural enhancement in sarcoidosis
The pattern of contrast enhancement may offer some clues as to whether one is dealing with an ischemic or non-ischemic process. In ischemic disease contrast enhancement begins subendocardially and spreads transmurally toward the epicardial surface. The enhancement also occurs in a distrubution corresponding to a known coronary artery territory. Conversely, contrast enhancement in non-ischemic heart disease is often located in the mid-wall of the ventricle and may be patchy or multifocal in nature.
Advanced Discussion (show/hide)»
Note: the above descriptions of various cardiac pathologies are overly simplistic and designed primarily for non-physicians.
Delayed gadolinium enhancement has become a primary diagnostic tool for detecting ischemic heart disease, including myocardial infarction, scar, and fibrosis. In nonischemic cardiac disease, however, contrast enhancement may be patchy or subtle, and often difficult to distinguish from that of the normal heart. Direct measurements of myocardial T1 and extracellular volume (ECV) offer a means to detect and quantify diffuse fibrosis and other infiltrative myocardial diseases.
For workup of possible intracardiac thrombus, contrast-enhanced imaging at 1-3 minutes is commonly used. Thrombus does not enhance and will appear dark against the bright blood pool background. The TI should be set to approximately 460 ms at 1.5T, or even higher if the heart rate is decreased.
Doltra A, Amudsen BH, Gebker R, et al. Emerging concepts for myocardial late gadolinium enhancement MRI. Curr Cardiol Rev 2013; 9:185-190.
Juan LJ, Crean AM, Wintersperger BJ. Late gadolinium enhancement imaging in assessment of myocardial viability. Techniques and clinical applications. Radiol Clin N Am 2015; 53:397-411.Kim RJ, Fieno DS, Parrish TB, et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation 1999; 100:1992-2002. (hyperenhancement corresponds to extent of myocyte necrosis and scar in myocardial infarction).
Kim RJ, Wu E, Rafael A, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med 2000; 343:1445-53. (reversible myocardial dysfunction can be identified with CE MRI before revascularization)
Moon J. Late gadolinium imaging quiz. Society of Cardiovascular Magnetic Resonance, 2007. (Answers to quiz are at this link)
So many gadolinium contrast agents are now available. What are the differences among them?
What is the best way to see myocardial enhancement?

