Immediately after hemorrhage begins, an expanding hematoma contains liquid (plasma) and solid (cellular) elements similar in composition and MR properties to blood within the vascular system.
 Components of whole blood
Components of whole blood
Plasma is over 95% water with some dissolved proteins (albumin, globulins, fibrinogen) and lipids (cholesterol, triglycerides). These macromolecules give plasma its yellowish color and produce mild shortening of relaxation times. At 1.5T the T1 and T2 values of plasma are approximately 2300 and 400 msec, respectively.
The solid elements of fresh blood are primarily erythrocytes (red blood cells, RBCs), with small contributions from leukocytes and platelets. Erythrocytes contain the oxygen-transporting, iron-containing protein hemoglobin (Hb). Hemoglobin may exist in several distinct chemical forms with markedly different magnetic properties. The state of Hb is thus a powerful determinant of the MR appearance of the solid portions of hematomas at all stages.
The solid elements of fresh blood are primarily erythrocytes (red blood cells, RBCs), with small contributions from leukocytes and platelets. Erythrocytes contain the oxygen-transporting, iron-containing protein hemoglobin (Hb). Hemoglobin may exist in several distinct chemical forms with markedly different magnetic properties. The state of Hb is thus a powerful determinant of the MR appearance of the solid portions of hematomas at all stages.
|
In arterial blood, over 95% of hemoglobin is in the oxyhemoglobin (oxy-Hb) state, while less than 5% is deoxyhemoglobin (deoxy-Hb). In venous blood, oxy-Hb still predominates, though in a smaller ratio (venous oxy:deoxy ≈ 70:30.)
Oxy-Hb is weakly diamagnetic as the bonding of oxygen results in a configuration around the heme iron with no unpaired electrons. Deoxy-Hb, however, has 4 unpaired electrons per iron atom and is strongly paramagnetic.
|
The volume fraction of RBCs (hematocrit) within a hematoma is also important. In normal adults, the hematocrit of circulating blood is in the range of 40-50%, with variations by age, sex, and altitude. As RBCs in a developing hematoma settle by gravity and begin to stick together during clotting, the local hematocrit may increase to 90% or more. Increasing hematocrit has three effects:
- Decreased "free" water content, reducing T1, T2 and spin density
- Decreased extracellular space, restricting diffusion
- Increased concentration of Hb, potentiating T2/T2* paramagnetic shortening by deoxy-Hb
|
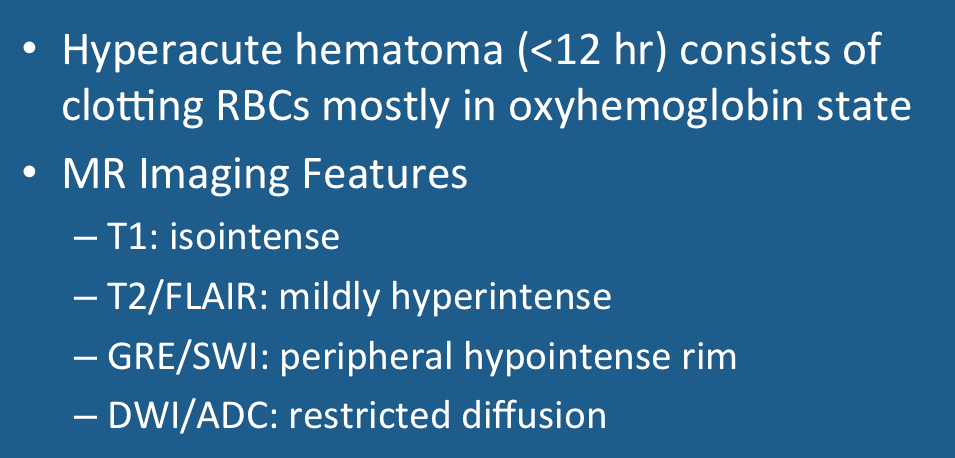
The hyperacute phase is often arbitrarily defined to be the first 12 hours after the onset of hemorrhage. Regardless of whether the blood source is arterial or venous, oxy-Hb will the dominant initial chemical species present. Clotting begins, and plasma is converted to serum as coagulation factors are consumed. Occasionally a peripheral halo of serum may be seen around the centrally contracting clot. Rarely, a RBC-serum fluid level may be observed before clotting is complete. Dexoy-Hb formation starts to occur around the hematoma's periphery.
|
As a result of these physical and chemical changes, a hyperacute cerebral hematoma is expected to have the following MR signal characteristics:
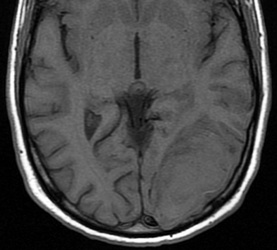
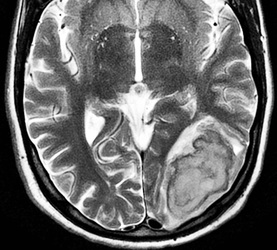
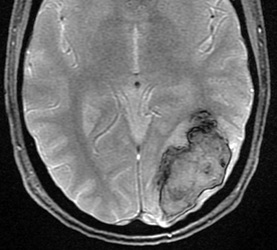
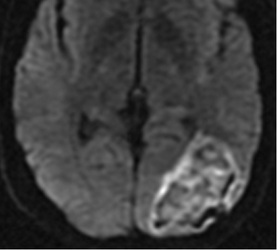
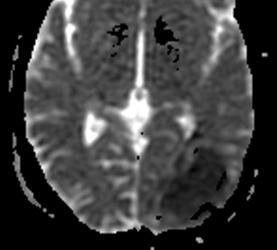
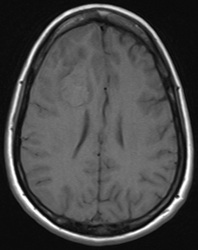
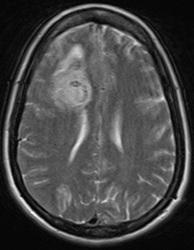
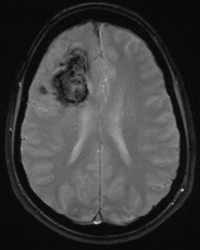
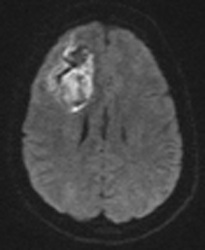
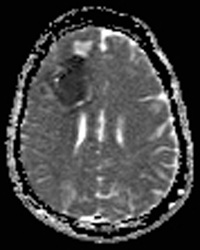
Above: Hyperacute cerebral hematoma imaged by CT and MR within 2 hours of ictus (click to enlarge images). The core of the hematoma is isointense to white matter on the T1-weighted image (top middle) and mildly hyperintense on the T2-weighted image (top right), representing oxy-hemoglobin. In the short interval between CT and MRI, some clot retraction has already occurred with a hyperintense peripheral halo on the T2-weighted image likely representing serum. Even at this early stage, some transition to deoxyhemoglobin formation has occurred rim hypointensity on the GRE image (bottom left). DWI (bottom center) and ADC image (bottom right) show restricted diffusion in the hematoma center due to reduced extracellular space and increased viscosity.
Below: Hyperacute cerebral hematoma imaged at 6 hours. Similar findings to case above, but more clot retraction and transition to deoxy-Hb has occurred.
Important Note: The discussion above primarily applies to higher field (≥ 0.5 T) systems where imaging findings are dominated by the paramagnetic effects of hemoglobin. At low and intermediate fields some important differences in imaging appearances are noted. See this Q&A for a more detailed analysis.
Advanced Discussion (show/hide)»
No supplementary material yet. Check back soon!
References
Atlas SW, Thulborn KR. MR detection of hyperacute parenchymal hemorrhage of the brain. AJNR Am J Neuroradiol 1998; 19:1471–1477.
Barth M, Moser E. Proton NMR relaxation times of human blood samples at 1.5T and implications for functional MRI. Cell Mol Biol 1997; 43:783-792.
Gomori JM, Grossman RI. Mechanisms responsible for the MR appearance and evolution of intracranial hemorrhage. Radiographics 1988; 8:427-440.
Linfante I, Llinas RH, Caplan LR, Warach S. MRI features of intracerebral hemorrhage within 2 hours from symptom onset. Stroke 1999; 30:2263-2267.
Vidmar J, Sersa I, Kralj E, et al. Discrimination between red blood cell and platelet components of blood clots by MR microscopy. Eur Biophy J 2008; 37:1235-40. (Areas of clots rich in platelets and high hematocrit >80% RBC have shorter T1 values.)
Atlas SW, Thulborn KR. MR detection of hyperacute parenchymal hemorrhage of the brain. AJNR Am J Neuroradiol 1998; 19:1471–1477.
Barth M, Moser E. Proton NMR relaxation times of human blood samples at 1.5T and implications for functional MRI. Cell Mol Biol 1997; 43:783-792.
Gomori JM, Grossman RI. Mechanisms responsible for the MR appearance and evolution of intracranial hemorrhage. Radiographics 1988; 8:427-440.
Linfante I, Llinas RH, Caplan LR, Warach S. MRI features of intracerebral hemorrhage within 2 hours from symptom onset. Stroke 1999; 30:2263-2267.
Vidmar J, Sersa I, Kralj E, et al. Discrimination between red blood cell and platelet components of blood clots by MR microscopy. Eur Biophy J 2008; 37:1235-40. (Areas of clots rich in platelets and high hematocrit >80% RBC have shorter T1 values.)
Related Questions
What are the different forms of hemoglobin and why do they have different magnetic properties?
What are the different forms of hemoglobin and why do they have different magnetic properties?