|
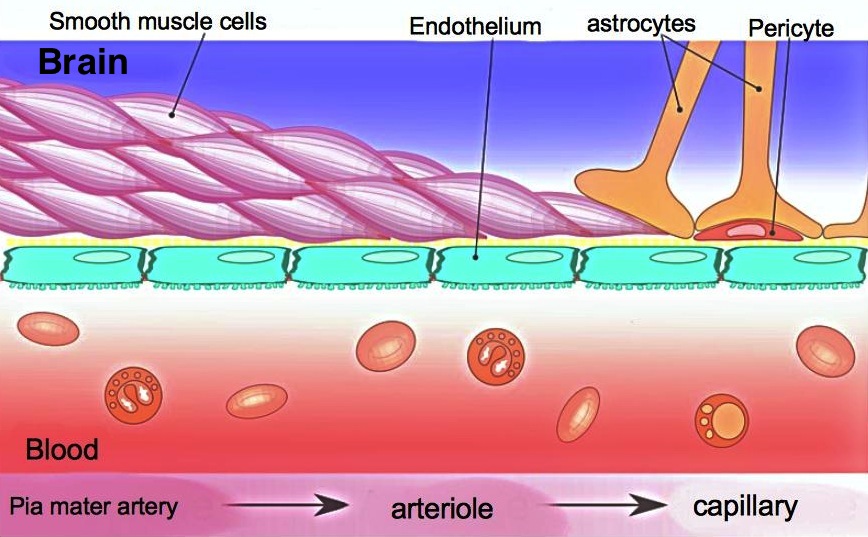
Gadolinium-containing contrast agents do not normally enter the extracellular spaces of the brain and spinal cord, being excluded by the blood-brain barrier (BBB). The BBB is formed by tight junctions between endothelial cells, allowing movement of only ions and small molecules (like O2) across the vessel wall. If the BBB becomes disrupted by disease (such as malignant tumors and infections), contrast agents will leak into the brain parenchyma producing T1 shortening and enhancement.
|
Accumulation of contrast in tissue due to a leaky BBB violates a fundamental assumption of the simple tracer kinetic model on which DSC imaging is based — that no pooling or retention of contrast agent occurs. In the presence of BBB disruption, blood flow/volume estimates may be significantly in error.
Two effects of T1-shortening due to gadolinium accumulation confound DSC perfusion imaging:
- Blunting of T2* signal loss. DSC methods rely on decreased signal due to T2*-dephasing during passage of the gadolinium bolus. Extravascular gadolinium increases signal due to T1 effects and may blunt this desired T2* shortening. In some cases a paradoxical post-bolus signal overshoot may occur.
- Effect on steady-state signal. DSC image acquisition is typically performed using relatively short TR values (1000-2000 ms typical). Areas with T1 shortening due to accumulated gadolinium will recover more quickly between RF-pulses and thus have higher steady-state signals. This phenomenon increases with higher flip angles (α).
Several strategies exist to compensate for gadolinium extravasation. One popular method is to administer a gadolinium "preload" of approximately ¼ to ⅓ of the total dose about 5-10 minutes before the regular injection and DSC sequence. The gadolinium preload raises the baseline signal in areas of contrast enhancement so that T2* changes during the DSC bolus can be better appreciated.
A second method to reduce T1 effects from gadolinium leakage is to reduce the RF-flip angle of the DSC acquisition sequence. Reduction of flip angle can only be taken so far, however, as signal-to-noise will also decrease. Other methods to compensate for gadolinium accumulation include software-based leakage correction algorithms.
A second method to reduce T1 effects from gadolinium leakage is to reduce the RF-flip angle of the DSC acquisition sequence. Reduction of flip angle can only be taken so far, however, as signal-to-noise will also decrease. Other methods to compensate for gadolinium accumulation include software-based leakage correction algorithms.
Advanced Discussion (show/hide)»
No supplementary material yet. Check back soon!
References
"Blood-brain Barrier", Wikipedia, The Free Encyclopedia.
Boxerman JL, Prah DE, Paulson ES, et al. Gadolinium-based cerebral blood volume estimation determined by comparison with MION as a criterion standard. AJNR Am J Neuroradiol 2012; 33:1081-87.
Boxerman JL, Schmainda KM, Weisskoff RM. Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. AJNR Am J Neuroradiol 2006; 27:859-67.
Welker K, Boxerman J, Kalnin A, et al. ASFNR recommendations for clinical performance of MR dynamic susceptibility contrast perfusion imaging of the brain. AJNR Am J Neuroradiol 2015; 36: E41-E51.
"Blood-brain Barrier", Wikipedia, The Free Encyclopedia.
Boxerman JL, Prah DE, Paulson ES, et al. Gadolinium-based cerebral blood volume estimation determined by comparison with MION as a criterion standard. AJNR Am J Neuroradiol 2012; 33:1081-87.
Boxerman JL, Schmainda KM, Weisskoff RM. Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. AJNR Am J Neuroradiol 2006; 27:859-67.
Welker K, Boxerman J, Kalnin A, et al. ASFNR recommendations for clinical performance of MR dynamic susceptibility contrast perfusion imaging of the brain. AJNR Am J Neuroradiol 2015; 36: E41-E51.