|
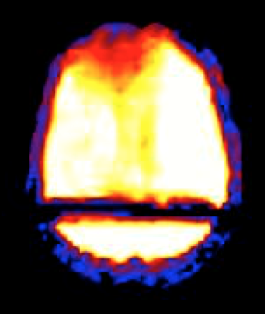
More severe and random errors (such as the gradient malfunction shown right) may be identified by outlier analysis, where differences between control and tagged data are discarded when exceeding certain predefined thresholds. Oval "masks" are commonly generated to exclude out-of-brain voxels. Statistical techniques using independent component analysis may be applied to further reduce noise.
|
 PD calibration image
PD calibration image
Advanced Discussion (show/hide)»
Here F is the blood flow rate, T1 is the longitudinal relaxation time of tissue in the absence of flow or exchange, MT0 is the tissue magnetization under fully relaxed conditions, and Ma and Mv are the time-dependent arterial and venous longitudinal magnetizations respectively.
Assuming the blood-tissue interaction occurs in a single, well-mixed compartment, the magnetization of venous blood exiting the system Mv = MT/λ, where λ is known as the blood-tissue partition coefficient, the fraction of labeled arterial water extracted during passage through the tissue. For brain, the value of λ is generally taken to be about 0.9, an average of gray and white matter obtained from [15O]water-labeled PET studies.
With continuous and complete inversion of arterial spins, the subsequent sampling of MT results in an exponential decrease in MT with an apparent time constant T1app, given by
Several assumptions are implicit in the Buxton model, any of which may be rightfully challenged in part:
- Perfect "plug" flow. The labeled magnetization enters as a perfect rectangular bolus with sharp leading and trailing edges. The arterial input function, a(t), is therefore zero except during passage of the bolus, where it takes the form a(t) = αe−t/T1b, where T1b is the relaxation time of blood. (In real life such a perfect rectangular spin-labeling profile is difficult to achieve, even with techniques like QUIPSS to improve edge definition of the bolus. Having a range of transit times leads to underestimation of blood flow.)
- Single compartment kinetics. All labeled water flowing into a voxel instantaneously exchanges into the tissue, a "well-mixed" condition. (However, some labeled spins remain in vessels before being exchanged while others flow out of the imaged slice without exchanging. Both effects lead to an underestimation of perfusion). The true extraction fraction (λ) needs to be measured or estimated, which for human brain tissue at normal flow rates is about 0.9. The usual form of the residue function in the Buxton model is given by R(t) = e−Ft/λ.
- Magnetization decay rate reflects tissue T1. As a consequence of assumptions 1 & 2 above, the magnetization relaxation function is assumed to have the form m(t) = e−t/T1t, where T1t is the tissue T1. (Because it ignores flow-though, magnetization transfer effects, and imperfect mixing, this assumption leads to in an overestimation of perfusion).
Alsop DC, Detre JA, Gola X, et al. Recommended implementation of arterial spin-labeled
perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med 2015; 73:102-116.
Buxton RB, Frank LR, Wong EC, et al. A general kinetic model for quantitative perfusion imaging with arterial spin labeling. Magn Reson Med 1998; 40:383-396.
Herscovitch P, Raichle ME. What is the correct value for the brain-blood partition coefficient for water? J Cereb Blood Flow Metab 1985; 5:65-69. (Answer: probably about 0.90 ml/g)
Mutsaerts HJMM, Steketee RME, Heijtel DFR, et al. Inter-vendor reproducibility of pseudo-continuous arterial spin labeling at 3 Tesla. PLOS One 2014; 9(8):e104108.
Petersen ET, Lim T, Golay X. Model-free arterial spin labeling quantification: approach for perfusion MRI. Magn Reson Med 2006; 55:219-232. (QUASAR method)
Petersen ET, Zimine I, Ho Y-C L, Golay X. Non-invasive measurement of perfusion: a critical review of arterial spin labelling techniques. Br J Radiol 2006; 79:688-701.
Pinto J, Chappell MA, Okell TW, et al. Calibration of arterial spin labeling data — potential pitfalls in post-processing. Magn Reson Med 2020; 83:1222-1234.
Wang Z. Arterial spin labeling perfusion MRI signal processing toolbox (ASLtbx). Version 1, May 2012. (manual for a freely available MATLAB-based toolbox for processing ASL data).
Williams DS, Detre JA, Leigh JS, Koretsky AP. Magnetic resonance imaging of perfusion using spin inversion of arterial water. Proc Natl Acad Sci USA 1992; 89:212-216. (derives modified Bloch equations to account for inflow of inverted spins)
Wong EC. Quantifying CBF with pulsed ASL: technical and pulse sequence factors. J Magn Reson Imaging 2005; 22:727-731.
How is the arterial input function used to extract more quantitative flow information from the DSC data?
How should imaging parameters be chosen to optimize an ASL acquisition?